RESEARCH SPOTLIGHT: Using Magnetic Resonance Elastography (MRE) To Define The Shear Properties Of Fat Under Load
We know that you have heard of MRI, but have you heard of MRE? Magnetic resonance elastography, or MRE as it is commonly known as, is an emerging MR technique that allows the stiffness of internal tissues to be measured quickly and noninvasively.
Researchers at NeuRA, led by Professor Lynne Bilston, have recently published a NeuRA Imaging study that define for the first time, the load dependent properties of in vivo adipose tissue (fat).
Palpation as an evaluation of tissue stiffness has long been the physician’s first indication of pathology, and MRE provides a formal mapping of these properties. The technique uses a source of shear vibration (similar in feeling to an electric toothbrush or mobile phone) and the MRI scanner is used to take pictures as the vibration travels through the soft tissues of the body. How quickly the wave travels and how fast it attenuates (is absorbed by the tissue), allows the stiffness of the tissue to be measured.
MRE has been used throughout the human body to measure the in vivo viscoelastic properties of healthy brain, liver, pancreas, kidney, heart, prostate, breast tissue, muscle, and increasingly to identify pathological changes in these tissues resulting in altered stiffness, such as the presence of tumours or liver fibrosis.
The stiffness of the soft tissues of the human body change under load, in a way that varies with the magnitude of the applied force. For instance, muscle that is passively stretched stiffens increasingly with the amount of stretch applied (think of your calf muscles as you reach progressively for your toes). The load-dependent properties of in vivo tissues are termed their “large deformation properties”, and comprehensive measurement of these properties, ideally in humans in vivo, are essential for biomechanical modelling, pre-operative surgical planning, and in the study of impact and pathology biomechanics.
Human adipose tissue (fat) is present subcutaneously (under the skin) over large portions of the body, and deforms substantially under normal everyday loading (think compression during sitting) and during impact. Accurate data on the strain-dependent stiffness of fat is essential for the creation of accurate biomechanical models.
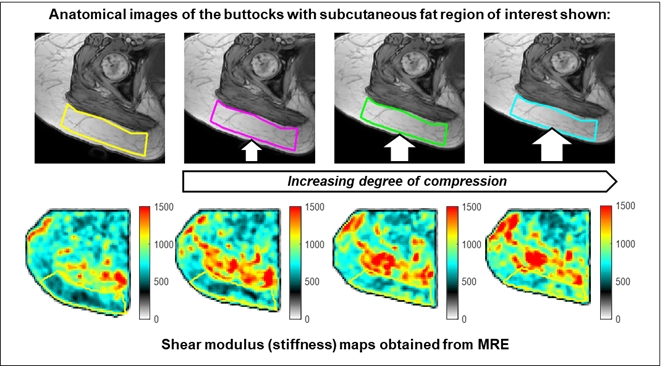
In this study, we combined static compression of a large deposit of subcutaneous fat – the buttocks – with MRE, to map the large deformation properties of fat. An example of the stiffness maps obtained from the study can be seen above, with the (light grey) subcutaneous fat region visible by the coloured rectangle, with the (dark grey) muscle region above it.
The key findings of the study include that:
- Static compression of human adipose tissue (fat) results in an increase in stiffness, in an exponentially increasing relationship.
- The baseline stiffness of fat was significantly lower than that of muscle.
- The relationships defined in this study (link below) can be used to develop physiologically realistic computational models for impact, injury and biomechanical modelling.
Full details of the published study, published in the Journal of the Mechanical Behavior of Biomedical Materials, can be found here:
https://www.sciencedirect.com/science/article/pii/S1751616123002771
The authors acknowledge the facilities and scientific and technical assistance of NeuRA Imaging, a node of the National Imaging Facility, a National Collaborative Research Infrastructure Strategy (NCRIS) capability.
Recent Comments